Screen 1 billion people to save 10 million lives by 2030.

Jan 09, 2025
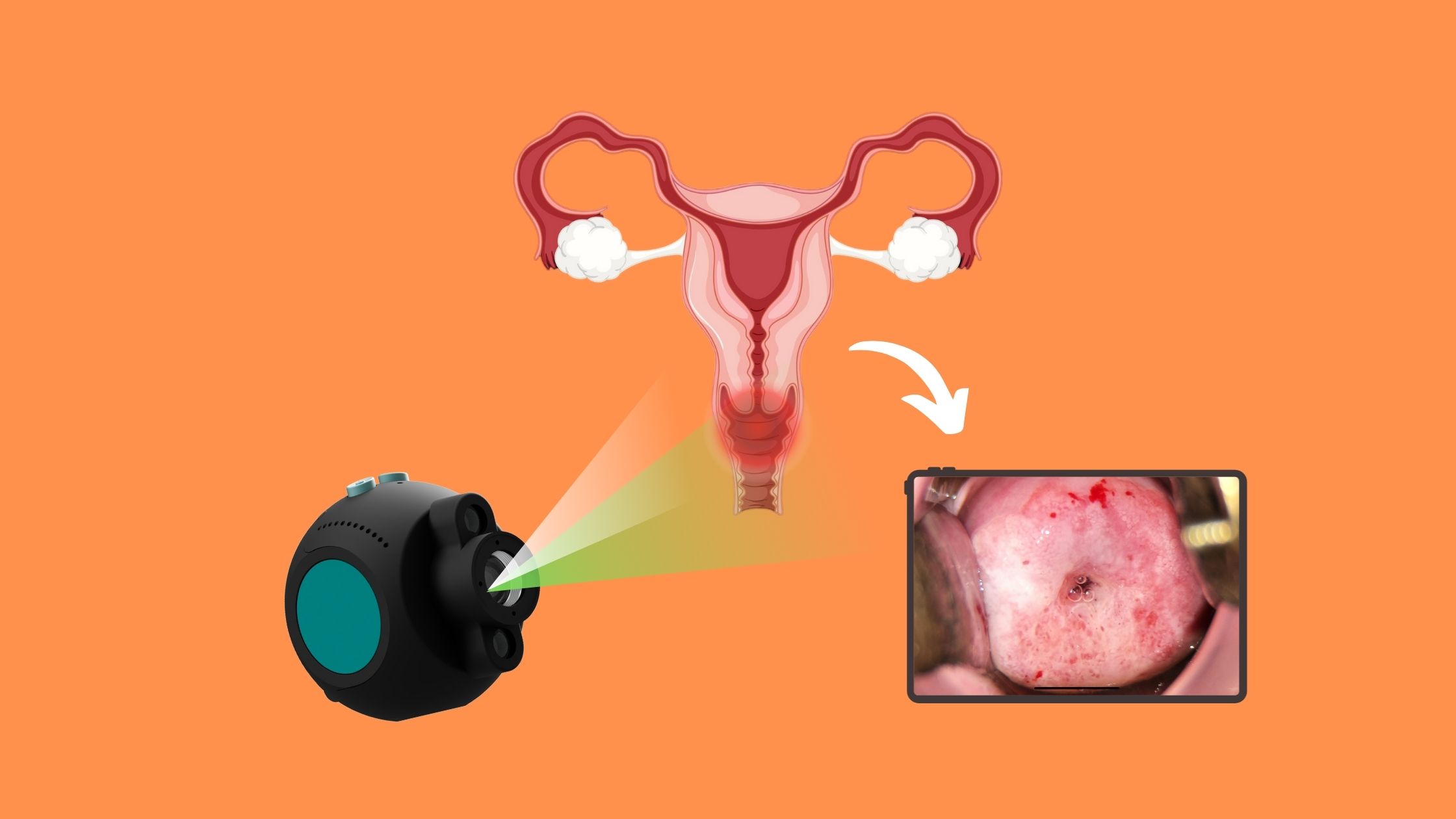
Colposcopy: A Key to Early Detection
Taking care of your cervical health is essential for your overall well-being, and regular screenings play an important role in early detection. Among these, colposcopy is a highly effective procedure for identifying potential issues. Unlike a routine Pap smear, colposcopy provides a closer and more detailed examination of your cervical health.
This blog will walk you through everything you need about colposcopy—what it is, why it matters, and how advancements like the nGyn technology improve the experience and outcomes.
Read more
What Is Colposcopy?
Colposcopy is a specialized procedure that allows doctors to examine your cervix, vagina, and vulva using a magnifying device called a colposcope. It’s typically recommended when a Pap smear or HPV test reveals abnormal results. Magnifying the cervical tissue helps doctors detect abnormalities requiring further testing or treatment.How to Prepare for a Colposcopy
Preparation is simple but essential. Your doctor may advise you to avoid sexual intercourse, vaginal creams, or medications for a day or two before the procedure. It’s also best to schedule your appointment when you’re not menstruating, as this ensures better visibility during the exam.Steps of the Colposcopy Procedure
During the procedure, you’ll lie on an exam table with your feet in stirrups, similar to a pelvic exam. A speculum is gently inserted to open the vaginal canal for a clear view of the cervix.- Applying Acetic Acid: A vinegar-like solution is applied to the cervix. This temporarily turns abnormal cells white, making them easier to spot.
- Examining with a Colposcope: The doctor uses a Colposcope to obtain a detailed, magnified view of your cervix and identify any areas of concern.
- Performing a Biopsy (if needed): If abnormal areas are detected, a small tissue sample may be taken for further analysis. While this might cause mild discomfort, a local anesthetic can help minimize pain.
Benefits of Colposcopy
Colposcopy offers several key benefits:
- Early detection of cervical abnormalities can prevent serious health issues.
- The magnified view of cervical tissue enables a precise diagnosis.
- It is a safe and generally painless experience for most patients.
Advancements in Technology: nGyn Colposcopy
Modern technology has significantly enhanced the colposcopy procedure, with innovations like the nGyn system setting new standards. The nGyn system provides:- Digital Imaging: High-resolution images for more accurate detection.
- Improved Diagnostic Accuracy: Reducing the need for unnecessary follow-ups.
- Enhanced Patient Comfort: A smoother, more efficient process that minimizes stress.
Reference:
- Massad LS, Einstein MH, Huh WK, Katki HA, Kinney WK, Schiffman M, et al. 2012 Updated Consensus Guidelines for the Management of Abnormal Cervical Cancer Screening Tests and Cancer Precursors. J Low Genit Tract Dis. 2013;17(5):S1-S27.
- Martin-Hirsch PP, Jarvis G, Kitchener H, Lilford R. Prophylactic antibiotics to prevent pelvic infection after diagnostic uterine procedures. Cochrane Database Syst Rev. 2000;(4): CD001357.
- Wentzensen N, Massad LS, Mayeaux EJ, Khan MJ, Waxman AG, Einstein MH, et al. Evidence-Based Consensus Recommendations for Colposcopy Practice for Cervical Cancer Prevention in the United States. J Low Genit Tract Dis. 2017;21(4):216-222.
- Huh WK, Ault KA, Chelmow D, Davey DD, Goulart RA, Garcia FA, et al. Use of primary high-risk human papillomavirus testing for cervical cancer screening: interim clinical guidance. Obstet Gynecol. 2015;125(2):330-337.
- Stuebs FA, Schulmeyer CE, Mehlhorn G, Ackermann J, Mehlhorn U, Renner SK. Impact of colposcopy in diagnosis and treatment of cervical intraepithelial neoplasia. Anticancer Res. 2018;38(1):345-350.
- Perkins RB, Guido RS, Castle PE, Chelmow D, Einstein MH, Garcia F, et al. 2019 ASCCP Risk-Based Management Consensus Guidelines for Abnormal Cervical Cancer Screening Tests and Cancer Precursors. J Low Genit Tract Dis. 2020;24(2):102-131.
- Wright TC, Massad LS, Dunton CJ, Spitzer M, Wilkinson EJ, Solomon D. 2006 Consensus Guidelines for the Management of Women with Cervical Intraepithelial Neoplasia or Adenocarcinoma in Situ. J Low Genit Tract Dis. 2007;11(4):223-239.
- Kitchener HC, Canfell K, Gilham C, Sargent A, Roberts C, Desai M, et al. The clinical effectiveness and cost-effectiveness of primary human papillomavirus cervical screening in England: extended ARTISTIC randomized trial cohort follow-up through three screening rounds. Health Technol Assess. 2014;18(23):1-196.
- Kyrgiou M, Koliopoulos G, Martin-Hirsch P, Arbyn M, Prendiville W, Paraskevaidis E. Obstetric outcomes after conservative treatment for intraepithelial or early invasive cervical lesions: systematic review and meta-analysis. Lancet. 2006;367(9509):489-498.
- Franco EL, Cuzick J, Hildesheim A, de Sanjosé S. Chapter 20: Issues in planning cervical cancer screening in the era of HPV vaccination. Vaccine. 2006;24:S171-S177.

Jan 01, 2025
Why Every Woman Should Prioritize Cervical Cancer Screening
Every Life Matters: A Story of Hope
Imagine preventing a life-threatening illness with a simple, routine test. That’s precisely what happened to a woman who never expected her life to take a sudden turn. During a routine cervical cancer screening, abnormal cells were detected early, giving her a second chance at life.
Stories like these are a powerful reminder that cervical cancer screening is not just about detecting illness—it’s about empowering women to take control of their health. Did you know cervical cancer is one of the top cancers affecting women worldwide?
Every year, countless lives are saved because women take the time to prioritize their health. The question is: will you be one of them?
Read more
What Every Woman Needs to Know About Cervical Cancer
Cervical cancer starts in the cells of the cervix, the lower part of the uterus that connects to the vagina. While it might seem far removed from everyday concerns, cervical cancer is primarily caused by the human papillomavirus (HPV), a common infection that many people contract at some point in their lives. The good news is that not all HPV infections lead to cancer. However, certain high-risk strains can cause changes in cervical cells, which, if undetected, may develop into cancer over time. Regular screening is essential—it identifies these changes before they become life-threatening.How Cervical Cancer Screening Saves Lives
Early detection is the key to successful treatment, and that’s where screenings come in. Pap smears and HPV tests are two essential tools in identifying cervical abnormalities early. A Pap smear looks for changes in cervical cells that could develop into cancer, while an HPV test identifies the high-risk strains of the virus that are most likely to cause these changes. Together, these tests form a powerful line of defense, catching potential problems before symptoms even appear.How Colposcopy Plays a Vital Role in Your Cervical Health
If a Pap smear or HPV test shows abnormal results, your doctor may recommend a colposcopy. This procedure uses a specialized instrument to take a closer look at your cervix, allowing for precise identification of any suspicious areas. Colposcopy is more than just a diagnostic tool—it’s a crucial step in cervical cancer prevention. By visualizing the cervix in detail, doctors can decide on the most effective treatment plan, ensuring no potential issue goes unnoticed. Thanks to advancements like the nGyn colposcopy system, the process is now more accurate and comfortable than ever. This innovative technology is designed to provide clearer images and better results, giving women the confidence they need to take charge of their health. 3 Key Reasons to Schedule Your Screening Today- Early Detection Saves Lives: Regular screenings catch abnormalities before they turn into cancer.
- The Process is Simple and Quick: A few minutes could protect your future.
- Empowerment Through Knowledge: Knowing your health status helps you make informed decisions.
- If you’re between 21 and 29, a Pap smear every three years is recommended.
- Between 30 and 65, you can opt for a Pap smear and HPV test every five years or continue with a Pap smear every three years.
- After 65, you may no longer need screening if your previous results were normal, but always consult your doctor.
Taking the First Step Toward a Healthier Future
Your health is worth prioritizing. Schedule your cervical cancer screening today—it’s a simple step with life-saving potential. And don’t keep this information to yourself. Please share this article with the women in your life because, together, we can spread awareness and save lives. By prioritizing cervical cancer screening, you’re not just protecting yourself but inspiring others to do the same. Let’s make cervical cancer a thing of the past—one screening at a time.References
- Arbyn M, et al. "Burden of cervical cancer and role of screening." Int J Cancer. 2020;146(4):776-786.
- Saslow D, et al. "American Cancer Society guideline for cervical cancer screening." CA Cancer J Clin. 2020;70(4):321-346.
- Wentzensen N, et al. "Use of colposcopy for cervical cancer prevention." Obstet Gynecol Clin North Am. 2013;40(2):207-220.
- World Health Organization. "Cervical cancer." WHO Fact Sheet. 2023.
- U.S. Preventive Services Task Force. "Cervical Cancer: Screening." JAMA. 2021;325(7):675-689.
Dec 19, 2024
How nGyn’s AI-Powered Colposcopy Is Changing Women’s Healthcare
Colposcopy is important for women's health because it detects cervical issues early, potentially preventing cervical cancer. Traditional colposcopy procedures have been found useful. However, they have limits in terms of vision and diagnostic accuracy. Recent advances in medical technology, particularly digital solutions, have greatly improved these treatments. nGyn's new approach to colposcopy is a major step forward in gynecological care.
Read more
What Makes nGyn a Game-Changer in Colposcopy?
nGyn uses advanced digital imaging and AI-powered tools to provide a clearer view of cervical tissues. Unlike older methods that only use optical magnification, nGyn provides high-resolution images in real-time, making it easier to spot problems. This technology also makes procedures quicker and more comfortable for patients, making it a top choice for gynecological exams.Benefits of Using nGyn for Colposcopy
- Clearer View: High-resolution images let doctors see cervical tissues in more detail.
- Smart Accuracy: AI helps recognize and map problem areas, giving more reliable results.
- Patient Comfort: Shorter, less invasive procedures make patients feel more at ease.
- Efficient Workflow: Digital tools simplify record-keeping and fit easily into existing healthcare systems.
How nGyn Improves Accuracy in Gynecological Exams
nGyn’s AI technology is a key feature. It reviews images to find minor problems that can be hard to see with the human eye. This approach gives doctors clear and detailed information, making diagnoses more accurate. Studies show that nGyn helps detect precancerous changes earlier, allowing timely treatment and better patient results.Integrating nGyn into Clinical Practice
Using nGyn in clinics Helping with :- Training Doctors: Teaching them how to use nGyn’s advanced tools effectively.
- Educating Patients: Explaining the process to help them feel comfortable and cooperative.
- Smooth Setup: Ensuring nGyn integrates easily with existing systems for a hassle-free start.
The Future of Gynecological Care with nGyn
nGyn’s potential goes beyond cervical screenings. Researchers are looking into how it can help with:- Pelvic Exams: Offering better visuals and diagnostics.
- Other Conditions: Finding issues beyond the cervix.
Conclusion
nGyn is changing how colposcopies are done, setting a new standard in women’s healthcare. Combining digital imaging and AI improves accuracy, comfort, and efficiency. Clinics worldwide should consider adopting nGyn to provide better care and outcomes for women.References
Smith, J. (2023). Advancements in Colposcopy Technology. Journal of Gynecological Imaging, 17(2), 45-58. Vancouver: MedTech Publications.
Nov 29, 2024
A Comprehensive Guide to Colposcopy for HPV-Positive Women
Colposcopy is a procedure used to look closely at the cervix, vagina, and vulva to detect any abnormalities when abnormalities are detected. The method is used to diagnose and treat pre-clinical and cervical cancer caused by human papillomavirus (HPV). For women who have tested positive for HPV, a colposcopy is essential in managing their health.
This comprehensive guide to colposcopy for HPV-positive women will cover the basics of the procedure, what to expect during the exam, and how to best prepare for the appointment. With the right information, women can be better informed and more confident in their choices regarding their health.
The nGyn colposcope will help examine the cervical screening with the imaging facilities, using white and green LEDs to see any abnormalities of the cervix. It will assist the doctor in giving the correct diagnosis to the patient.

Read more
What is colposcopy?
Colposcopy is a technique used to examine the cervix and other organs in the pelvic region. During a colposcopy, a doctor will examine the cervix using a magnifying instrument called a colposcope. This procedure is performed with the cervix covered with a testing solution called a colposcopic dye. The dye will stain the cells and make them easier to visualize. The colposcopic dye helps to check any more pronounced abnormalities, such as lesions. A colposcopy may be performed at the same time as a Pap.What is a Pap test?
A Pap test checks for cell changes that may turn into cervical cancer. A colposcopy is performed simultaneously with a Pap test to look for changes on the cervix that can’t be seen with the naked eye.What causes HPV?
HPV is a virus genus that affects both men and women equally. The virus usually causes no symptoms, and most people are unaware they have it. A person can have HPV for years and not know it. HPV can induce alterations in the cervix's cells, vulva, vagina, anus, and other body areas. These changes can lead to cancer over time. The types of HPV that cause warts on the hands and feet or rough spots on the lips differ from those of HPV that cause abnormal cell changes in the cervix. Not all types of HPV cause changes in cells. Many patients infected with the virus are unaware that they are infected, and their bodies fight off the infection. Some types of HPV are more likely to cause cancer than others. HPV 16 and HPV 18 are the two types most likely to cause cancer. HPV can cause cervical cancer in two ways: precancerous lesions and cervical cancer.
What is the purpose of a colposcopy?
A colposcopy is used to see the cervix and other areas of the pelvic region with a colposcope. It is a diagnostic procedure used to investigate abnormalities of the cervix and vulva. During a Pap test, the cervix and other parts of the pelvic area may seem abnormal. Still, more testing is required to identify whether these changes are due to cell abnormalities or irregularities on the mucosal surface. A colposcopy allows a doctor to examine the cervix and other areas of the pelvic region at a much higher magnification than a Pap test. Allows for better identification of abnormal cells and their locations. The colposcopy is also used to identify any microabrasions that may have occurred during a Pap test. During a Pap test, the cervix is either scraped or a small brush is used to collect cells. This can cause microabrasions on the cervix. Identifying them helps determine the best follow-up treatment.What to expect during the colposcopy appointment
Before the colposcopy begins, the woman may be asked to change into a gown and empty her bladder. The woman will most likely be asked to lie on her back with her hips elevated and her knees slightly open. The doctor may apply a unique solution known as an acetic acid solution to help image any abnormal areas. This solution is applied to the cervix using a cotton swab. The answer may sting or burn. It may temporarily turn the room a shade of white or yellowish-white. A colposcopy is a unique magnifying instrument that uses light. The doctor will use it to look at the cervix and other areas of the pelvic region. The woman may be asked to cough or bear down to better view the cervix. The doctor may take a sample of cells from the cervix. This sample is sent to a laboratory for testing.How to prepare for a colposcopy
Women should do their best to stay hydrated and eat healthy before a colposcopy. This can make the procedure less uncomfortable and speed up the healing process. Before the colposcopy, women should take a warm bath or use a warm heating pad to help relax the pelvic area. Some women find it helpful to reduce discomfort by taking a mild pain reliever or anti-inflammatory medicine before the colposcopy. Cleaning the vulva and surrounding area is recommended before the colposcopy. Wiping the area with warm water and a mild soap should suffice. It’s also a good idea to avoid wearing deodorant or scented hygiene products, especially if the skin is broken. Pregnant women should consult with their doctor about when to get a colposcopy.How to interpret results from a colposcopy
The results of a colposcopy may be reported as positive or negative. The doctor may recommend a repeat colposcopy in a few years if they are negative. This is an excellent time to ask about HPV vaccination. Suppose the results are positive (i.e., abnormal cells identified). In that case, the doctor may recommend the following.Follow-up treatments:
A follow-up colposcopy: If the abnormal cells were located on the cervix's surface or walls, the doctor might perform a follow-up colposcopy to investigate the findings further. If the abnormal cells were inside the cervix, the doctor might perform a cone or LLETZ biopsy. A cone biopsy: During this procedure, the doctor uses a small scalpel to remove the abnormal areas on the cervix. This minor procedure can be performed in the doctor’s office. The doctor may use a local anesthetic or prescribe pain medication to ease discomfort. LLETZ biopsy: During this procedure, the doctor uses a narrow wire loop to remove the abnormal areas on the cervix. The coil is heated to destroy the cells. This procedure is also performed in the doctor’s office and can be done with local anesthesia.Possible follow-up treatments for abnormal colposcopy results
If the colposcopy reveals abnormal cells, the doctor may recommend a follow-up treatment to remove the cells. Women who have had a colposcopy and have a positive result should consult their doctor to explain the findings and discuss the next steps toward a healthy cervix. Women with an abnormal Pap test or who have had a colposcopy and are found to have abnormal cells may be prescribed a short course of antibiotics. This reduces the risk of infection, which can cause the abnormal cells to multiply and spread. Women with positive colposcopy results may be prescribed a short course of HPV medications.What to do after a colposcopy
After a colposcopy, the tissue may look inflamed or bruised. The patient should keep the area clean with warm water and use a pad to catch any discharge. If the doctor performs a biopsy, the woman may experience pain and discomfort in the pelvic region. Taking over-the-counter pain medicines as prescribed can help manage discomfort. taking lots of rest and drinking plenty of water is essential for the body's recovery. Some spotting or bleeding might occur if the biopsy is performed on the cervix. This is common and will vanish in a few days or a week. It’s essential to keep the area clean and avoid sexual activity until the bleeding subsides.Colposcopy risks
While many women have a colposcopy with no complications, there is always a small risk of infection, bleeding, or injury to the urethra, bladder, or other nearby organs. In addition, the disease risk is higher when an acetic acid solution is used.nGyn Cervical Screening System:
The nGyn colposcope assists in obtaining accurate cervical diagnoses. Its prescribed workflow reduces subjectivity and variability in colposcopies. AI-powered diagnostics act as guidelines for decision-making, enhancing the accuracy of the procedure.References:
- Cooper DB, Dunton CJ. Colposcopy. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 [cited 2023 Oct 10]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK564514/
- Hospitals M. Best Hospitals in India | Medicover Hospitals. [cited 2023 Oct 10]. Colposcopy: a comprehensive guide for understanding. Available from: https://www.medicoverhospitals.in/articles/everything-you-need-to-know-about-a-colposcopy
- Burness JV, Schroeder JM, Warren JB. Cervical colposcopy: indications and risk assessment. Am Fam Physician. 2020 Jul 1;102(1):39–48.

Sep 02, 2024
Your Guide to Cervical Cancer Screening: Importance, Types, and Results
Cervical cancer screening is a critical preventive measure aimed at detecting abnormal cells in the cervix that could develop into cancer. The primary purpose of these screenings is to identify changes early, enabling timely treatment and increasing the chances of successful outcomes. Early detection is crucial, as it significantly improves the likelihood of treating cervical cancer effectively.
Read more
Types of Cervical Cancer Screening Tests
Pap Smear
- What it is: The Pap smear, or Pap test, involves collecting cells from the cervix to identify any precancerous or cancerous changes.
- How it is performed: During a pelvic exam, a healthcare provider uses a small brush or spatula to collect cells from the cervix gently.
- What results mean: Normal results indicate no abnormal cells were found. Abnormal results require further testing to determine the presence and severity of any abnormalities.lll
HPV Test
- What it is: The HPV test detects the presence of high-risk types of human papillomavirus (HPV) that can lead to cervical cancer.
- How it is performed: Similar to the Pap smear, cells are collected from the cervix and tested for HPV DNA.
- What results mean: A positive result indicates an HPV infection, which may necessitate additional monitoring or testing to prevent the development of cervical cancer.
Who Should Get Screened?
Age recommendations:
- Women aged 21 to 65 should undergo regular cervical cancer screening.
- Screening typically begins at age 21 with Pap smears every three years.
Frequency of screening:
- Women aged 30 to 65 can opt for Pap smears every three years, HPV testing every five years, or a combination of both every five years.
Risk factors necessitating more frequent screening:
- Women with a history of cervical cancer or pre-cancerous lesions
- Women with HIV infection, a weakened immune system, or DES exposure before birth
Preparing for a Cervical Cancer Screening Test
Pre-test guidelines:
- Avoid intercourse, douching, or using vaginal medications for 48 hours before the test.
- Schedule the test when you are not menstruating.
What to expect during the test:
- The test is typically quick and may cause mild discomfort but should not be painful.
- A healthcare provider will explain the procedure and answer any questions you may have.
Post-test care and follow-up:
- Follow any instructions provided by your healthcare provider.
- Await your results and schedule any necessary follow-up appointments.
Understanding Your Test Results
Normal results:
- Indicate no abnormal cells were detected. Continue regular screenings as recommended.
Abnormal results and what they mean:
- May indicate the presence of abnormal cells that require further evaluation.
- A follow-up colposcopy or biopsy may be recommended to examine abnormal areas more closely.
Follow-up procedures for abnormal results:
- Additional tests or treatments may be needed depending on the severity of the abnormalities.
The Role of Cervical Cancer Screening in Prevention
Cervical cancer screening is a powerful tool in preventing cervical cancer. Regular screening detects abnormal cells early, preventing them from developing into cancer. Statistics show a significant reduction in cervical cancer cases in populations with regular screening programs.Addressing Common Concerns and Myths
Common fears about screening:
- Some women fear the test will be painful or embarrassing. However, the procedure is generally quick and well-tolerated.
Debunking myths related to cervical cancer screening:
- Myth: "If I feel fine, I don't need a screening." Fact: Cervical cancer often has no symptoms in its early stages, making regular screenings vital.
Resources and Support for Patients
Where to get screened:
- Local health departments, clinics, and hospitals offer cervical cancer screening services.
References:
- Cervical cancer screening [Internet]. [cited 2024 Jul 18]. Available from: https://medlineplus.gov/cervicalcancerscreening.html
- Harsha Kumar H, Tanya S. A study on knowledge and screening for cervical cancer among women in mangalore city. Ann Med Health Sci Res [Internet]. 2014 [cited 2024 Jul 18];4(5):751–6. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4199169/
- Cervical cancer screening - nci [Internet]. 2022 [cited 2024 Jul 18]. Available from: https://www.cancer.gov/types/cervical/screening

